


A 53-year-old man presented to orthopaedic clinic with a 2-year history of severe unilateral heel pain and recent difficulty weight-bearing. Previous treatment for plantar fasciitis with physiotherapy, steroid injections and orthotics had been unsuccessful and prior radiographs and ultrasound had been reported as normal. An MRI was subsequently performed.
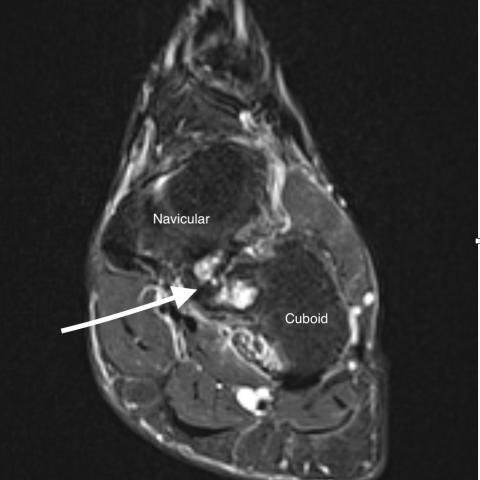
An MRI of the foot (Figs. 1-4) demonstrated an abnormal articulation between the posteromedial cuboid and plantolateral navicular bones. There was associated low T1 and high STIR signal with oedema and cystic change either side of the pseudo-articulation. The remainder of the foot and ankle had normal appearances with no imaging features of the clinically suspected plantar fasciitis. The MRI findings were consistent with a fibrocartilaginous cubonavicular coalition.
On retrospective review of a previous plain radiograph (Fig. 5), there is abnormal and irregular apposition of the cuboid and navicular bones with associated periarticular sclerosis but no osseous coalition.
Tarsal coalition is an abnormal union between two or more tarsal bones and is a rare, but im-portant, cause of chronic foot pain. Although often congenital, acquired causes include trauma, infection, arthritis and tumours [1]. Historically, the estimated prevalence was less than 1% [2] , however recent studies have suggested it could be as high as 11% [3].
Presentation is often non-specific and delayed until adolescence, when increased mechanical strain or direct impingement of surrounding structures leads to worsening pain. Given the lack of documentation in the literature, it is difficult to explain the delayed presentation in this case but we postulate it may due to the time taken to develop associated degenerative changes, as illus-trated by the articular cystic changes. Although often presenting with unilateral symptoms, up to 50% of case are bilateral [1]. Calcaneonavicular and talocalcaneal coalitions account for 90% of cas-es; Cubonavicular coalition represents less than 1%, with only a few documented cases [4]. It has been described as predominantly asymptomatic with an incidental diagnosis, however, as in this case, it can present with chronic, unremitting pain at rest as well as during activity [5].
Conservative management (immobility, orthotics and analgaesia) may be insufficient. Surgical in-terventions range from resection of the coalition to arthrodesis [4,5].
Three fundamental variations of coalition exist, based on the bridging tissue’s morphology: osse-ous (synostosis), cartilaginous (syndchondrosis) and fibrous (syndesmosis).
Plain radiograph findings can be subtle and often overlooked, particularly in non-osseous coalitions whose features include subchondral sclerosis, joint space narrowing and unusual articular orienta-tions. Well documented signs of the more common calcaneonavicular coalition (anteater nose sign) and talocalcaneal coalition (talar beak and C Signs) are still rarely identified [3]. The rarer coali-tions’ findings may be non-specific, often necessitating CT or MRI, where standard 3-plane acquisi-tions are usually sufficient [6].
In osseous coalitions, the fused articulation manifests as boney-bridging on CT and bone marrow contiguity on MRI. In non-osseous coalitions, CT is less useful due to the lack of structural change at the articulation. MR then helps to distinguish the different forms: Fibrous coalitions demonstrate loss of the fat plane between the tarsal surfaces with low signal on T1 and T2 weighted sequences; Cartilaginous coalitions will also show loss of the fat plane but will have intermediate T2/STIR signal with possible fluid signal change. Bone marrow oedema is frequently observed in all coalitions [6,7].
Although rare, cubonavicular coalition is an important differential for unexplained chronic foot pain.
Written patient consent for this case was waived by the Editorial Board. Patient data may have been modified to ensure patient anonymity.
Fibrocartilaginous cubonavicular coalition
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.




Based on the provided MR and X-ray images, a pronounced abnormality can be observed in the midfoot region anterior to the talus, mainly in the area between the cuboid and the navicular bones:
Based on the patient’s history of chronic heel/midfoot pain and the imaging findings, the following potential diagnoses are considered:
Considering the imaging findings, the most likely cause remains the relatively rare tarsal coalition between the navicular and the cuboid.
Taking into account the patient's clinical history (long-standing chronic foot pain with poor response to conventional treatment) and the MRI findings of atypical joint fusion and cystic changes, the diagnosis leans towards:
Cubonavicular Coalition
This type of tarsal coalition is uncommon and can result in chronic foot pain due to prolonged activity or weight-bearing.
For a confirmed cubonavicular coalition, the treatment and rehabilitation plan can be divided into the following steps:
Whether managed conservatively or postoperatively, a gradual increase in activity is recommended. The FITT-VP principle can be referenced:
If bone quality is suboptimal or there are coexisting cardiopulmonary issues, exercise intensity should be adjusted accordingly and individualized.
Disclaimer: This report provides a reference for medical analysis and does not replace in-person consultations or professional medical advice. Patients should consider their personal situations and seek guidance from a professional medical team for final diagnosis and treatment planning.
Fibrocartilaginous cubonavicular coalition